Not just you and the patient: Clinical health psychology support for your patients, their networks, you and your team
I don’t need to explain to any healthcare professional that physical health conditions, illness and injury have a psychological impact. The effect of a diagnosis that could be life-limiting or life-changing can touch every aspect of a patient’s life. Loved ones, family and friends can also struggle seeing someone they care about affected this way.
In aviation, we often talk about technical (flying the aircraft) and non-technical (managing people, responding to the unexpected) skills. I would strongly argue that’s a useful perspective in healthcare as well: Atul Gawande provides the best description of implementing this I have found so far (The Checklist Manifesto, Gawande, 2010). In this blog, I’m focussing on explaining how appropriate psychological support can improve well-being in patients with a life-limiting illness or illness or injury that requires significant adjustment and how psychological skills training can support healthcare professionals who need to have distressing conversations as part of their professional role.
Whether you work in Oncology or similar specialisms, the NICE guidance on developing and providing psychological, social and spiritual support for adults with cancer is an informative starting point. It’s available here: https://www.nice.org.uk/guidance/csg4/resources/improving-supportive-and-palliative-care-for-adults-with-cancer-pdf-773375005
In essence, this has been my starting point in Clinical Health Psychology since I began working in the area. It suggests events which should trigger psychological assessment (diagnosis, starting, during and finishing treatment, relapse and approaching death), appropriate approaches to support and appropriately emphasises the need to ensure that family and friends are supported as well. In my experience, the element I would add is that discharge with or without long-term surveillance should be a trigger point as well. I have found that the oncology and palliative care framework can be easily adapted to other conditions such as CFS/ME, cardiology and diabetes.
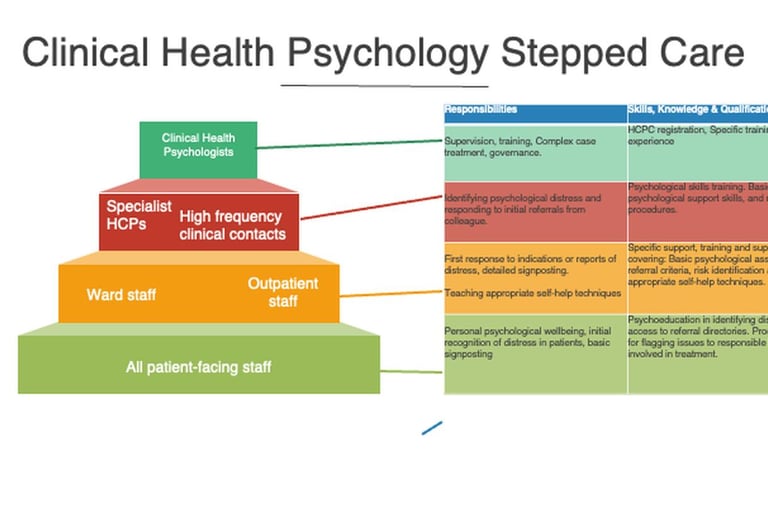
The other element of the NICE guidelines I particularly like is the concept that every professional in a healthcare setting who has any patient-facing role should be able to identify and respond to psychological distress. NICE suggest four levels which I typically summarise in a pyramid like the one below:
Fundamentally, this means it can’t be just you and the patient. It needs everyone involved to get the best outcome. In a primary care setting (I would include that in “high-frequency clinical contacts”) , that might mean empowering reception staff to flag distressed patients to the clinician they are about to see or teaching nursing staff to provide psychological support based on self-help techniques while being able to identify significant psychological risk and respond appropriately.
For healthcare professionals, clinical health psychology can provide training and supervision in psychological skills to enable the appropriate response and support.
For patients, clinical health psychology can support them and their loved ones in the face of the significant psychological challenges associated with frightening diagnoses or physical health conditions that require complex or long-term treatment or large adjustments. I talk about this in my parallel blog here: https://oaktreepsychology.com/its-not-all-in-the-mind-how-psychology-can-help-people-affected-by-physical-health-conditions
If you’d like to know about support and training for you and your team or referring your patients for psychological support, please do get in touch.